Scientists emulate human blood–retinal barrier on a microfluidic chip
The device contains living cells and mimics the structure and physiological conditions of the blood–retinal barrier; it also enables testing molecules in vitro and studying diseases such as diabetic retinopathy.
23/01/2018
For some years now, scientists have been researching in order to find ways of reducing animal testing and accelerating clinical trials. In vitro assays with living cells is an alternative, but has limitations as the interconnection and interaction between cells cannot be easily reproduced. To overcome this, scientists are developing systems that mimic tissues and organ functions in conditions very close to reality. These type of devices, called “Organ-on-a-chip”, include microenvironments and microarchitectures in order to emulate the living organs and tissues.
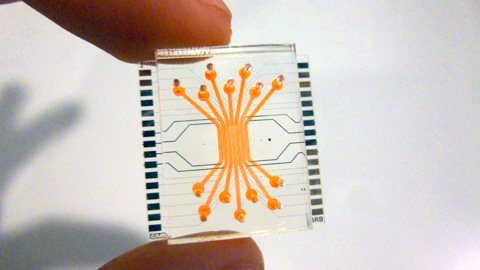
A team of scientists in Barcelona has developed a microfluidic device which mimics the human blood-retinal barrier. The scientists are from the Biomedical Applications Group of the Microelectronics Institute of Barcelona (IMB-CNM) of the Spanish National Research Council (CSIC), the CIBER-BBN, and from the Diabetes and Metabolism group of the Vall d’Hebron Research Institute (VHIR), CIBERDEM- Institute of Health Carlos III, and the Universitat Autònoma de Barcelona (UAB).
The study, featured on the cover of the journal “Lab-on-a chip”, is what experts technically call “proof of concept”, that is, it demonstrates the feasibility of the design imagined by the scientists.
Emulating the structure of the blood-retinal barrier
José Yeste, CSIC scientist at the IMB-CNM and at the Microelectronics and Electronics Systems Department at the UAB, and main author of the study, explains that the device is composed by several parallel compartments, arranged to emulate the retinal layer structure. In every compartment a type of cells has been cultured: endothelial cells (which constitute capillary vessels which carry oxygen and nutrients), neuronal cells (which form the neuroretina), and retinal pigmented epithelial cells, which form the outer layer of the blood-retinal barrier.
The compartments are interconnected by a grid of microgrooves under the cells, with which cells can exchange signal molecules and therefore communicate between them. As a result, substances produced by some cells can reach the other cells, generating cellular communication and interaction like in a living organ. Also, the device enables to expose endothelial cells to the particular mechanical conditions, like the ones induced by the blood stream.
As Rosa Villa, CSIC scientist and head of the Biomedical Applications Group, explains, “in the living organism, endothelial cells covering the inner walls of blood vessels are exposed to the mechanical stimulus of the blood stream. In the cell cultures where this condition is not reproduced, we could say the cells are 'sleepy' and do not react as they would do in real conditions”.
Rafael Simó, who leads the Diabetes and Metabolism group of the Vall d’Hebron Research Institute (VHIR) says: “The most relevant characteristic of this technology is that it mimics what happens ‘in vivo’ in the retina and therefore can be an essential tool to boost in vitro experimentation. On the device, the cells grow constantly when in contact with a fluid, as happens in the human retina. Also, the cells keep a close interaction between themselves by chemical mediators, which makes it possible to see what happens in one type of cell when another type of cell nearby is harmed. Also, it is possible to measure electrical resistance with which to assess the functionality of the retinal neurons”.
The scientists tested the correct formation of the blood-retinal barrier by assessing its permeability, its electrical resistance and the expression of proteins found in the tight junctions between cells, which are expressed when cells have established a barrier function.
The tests were designed to check whether the barrier was properly formed, but keeping the natural permeability to allow the pass of nutrients and oxygen, and to find out if the cells were in contact with each other and interacting.
This device, scientists say, can be used to study the effects of molecules or harming conditions on the human retina. The team also wants to use the device to study diabetic retinopathy, a disease whose causes and progression are not well understood yet.
Previously, the team lead by Rosa Villa at the CSIC Microelectronics Institute of Barcelona (IMB-CNM) had created a device which emulates the blood-brain barrier. They also developed a microfluidic chamber (Liver-on-a-chip) that mimics the hepatic microcirculation. In this case, they designed and manufactured the device together with scientists at the IDIBAPS.