Cellular Immunology
Research Lines

Protein autoantigens in type 1 diabetes - Dr. Dolores Jaraquemada
Regarding protein recognition by T cells, our approach, following our previous experience with T1D and other autoimmune diseases, is to find T cell ligands that are present in the periphery but not in the thymus. Thus, we seek to identify CD4+ and CD8+ T cell epitopes for which there is poor central tolerance. Our approach includes two steps:
Peptidome of pancreatic B cells. Comparison with thymic natural peptide repertoires. We aim to identify ex vivo peptides presented by MHC class I and class II molecules from pancreatic and thymic B cells from donors that match relevant MHC class I and II alleles. We will also analyze peptides presented by dendritic cells from healthy donors expressing T1D-associated HLA alleles pulsed with B cell protein extracts and/or soluble autoantigens. T cell reactivity to identified natural ligands will be examined.
Is there a differential repertoire of peptides presented by MHC-II molecules in the thymic cortex and medulla? Immunoproteomic analysis of the repertoire of peptides involved in positive and negative selection in the thymus after tissue microdissection. Searching for B cell-specific peptides identified in the thymic medulla.

Mitochondrial dysfunction and autoimmunity. Type 1 diabetes - Dr. Carme Roura-Mir
Lipid autoantigens in human type I diabetes
Insulin-specific autoreactive CD8+ and CD4+ T cells are key to driving the autoimmune response in type 1 diabetes. Other antigenic specificities may be equally important during the development or maintenance of the disease. Most of these proteins reside in the insulin secretory granules or crinophagic bodies of β-cells. There are some reports of MHC class I peptides presented in human T1D. Much less is known about the peptides recognized by CD4+ regulatory or effector T cells in human T1D.
Apart from proteins, lipid-based antigens can be loaded onto non-classical MHC-I CD1 molecules and recognized by NKT cells. Both exogenous and endogenous lipids have been shown to gain access to intracellular compartments and cross-link CD1 molecules. However, the target ligands recognized by these cells in the autoimmune context are barely known. Furthermore, little is known about the local lipid ligands for NKT cells that may be influencing the outcome of the disease. The group is working on two different aspects:
- The regulatory role of iNKT cells in type 1 diabetes
NKT cells regulate effector T cells in an IL13-dependent manner. In patients with T1D, NKT cells appear to lose their regulatory capacity, which may be associated with deficient IL13 production early in the disease. Usero et al. Diabetes 2016;65:2356–66.
The regulatory deficiency of NKT cells in patients with T1D may be related to a differential gene expression pattern compared to NKT cells from healthy controls (ongoing research).
- Lipid-based autoantigens recognized by iNKT cells in T1D
Due to their secretory function, B cells have a highly developed ER and are highly susceptible to ER stress. The group studies whether cellular stress alters the lipid content of B cells by generating lipid antigens that activate iNKT cells.
Response to lipid extracts from b cells

HLA peptides and antigen presentation - Dr. Iñaki Alvarez
Iñaki Alvarez's current research lines are:
- Study of the specificity and contribution of HLA peptide repertoires of different proteasomes and their role in tolerance and disease.
- Analysis of the role of the autoimmune regulator (AIRE) in antigen expression, processing and presentation.
- Study of standard and post-translationally modified HLA ligands in tolerance and disease.

Natural Killer Cells in cancer immunotherapy - Dr. Aura Muntasell
The team gathers researchers from Hospital del Mar Research Institute and Univ. Autònoma de Barcelona (UAB) being coordinated by Dr. Aura Muntasell (ORCID; https://orcid.org/0000-0003-2894-0486). Laboratories are located at the Barcelona Biomedical Research Park (PRBB) and at the Institut de Biotecnologia i Biomedina (IBB) premises.
The team has a broad and recognized experience in the study of human Natural Killer (NK) cell biology, involved in the immune response to certain microbial pathogens and tumors.
NK cells can recognize and eliminate transformed cells while facilitating the development of tumor-specific adaptive immunity by shaping the tumor microenvironment through the secretion of pro-inflammatory cytokines. Several mechanisms decreasing NK cell function had been described in cancer patients.
Cancer immunotherapy based on NK cells comprises a range of innovative strategies aimed at harnessing the natural potential of these immune system cells to fight cancer.
Research Lines:
Our current research lines include:
- Immunotherapy to enhance NK cells: Identification of target molecules that, can be leveraged with biological treatments to boost the function of NK lymphocytes in cancer patients.
- NK cells as biomarkers for oncological treatments: Study of NK cells as predictive indicators of response or resistance to treatments, specifically in patients with breast and colon cancer.
- Genetic engineering in NK cells: Development of NK lymphocytes resistant to the suppressive mechanisms of solid tumors as new approaches for adoptive cell therapy for cancer treatment.
- Adoptive cell therapy with NK lymphocytes: Development of protocols to optimize NK lymphocyte-based cancer cell therapy and patient monitoring.
Our research, builds on data from preclinical experimental systems and observational studies in collaboration with the Medical Oncology and Pathology Departments at Hospital del Mar.
Projects
Dual genetic engineering of NK cells for cancer immunotherapy (DUAL-NK). Aura Muntasell Castellví (PI). Convocatòria Consolidación Investigadora. AEI, Ministerio de Ciencia e Innovación. Execution: 1/04/24 → 30/06/26.
Development of a TGF-ß- and Activin A-Resistant off-the-shelf NK cell product for cancer treatment (TAR-NK-UABAura Muntasell Castellvi (PI). 2024PROD00086) Agència de Gestió d'Ajuts Universitaris de Recerca (AGAUR). Execution: 2/12/24 → 1/06/26.
Optimizing NK cell-based immunotherapy in HER2+ breast cancer. Aura Muntasell Castellví (PI, IMIM). FIS - Instituto de Salud Carlos III (ISCIII) Ref. PI22/00040. Execució: 1/01/23 → 31/12/25.
Immune cell communications in health and disease. Aura Muntasell Castellvi (Researcher, IMIM). Ajuts Grups de Recerca de Catalunya (Ref. 2021SGR00683_IMIM). Direcció General de Recerca de la Generalitat de Catalunya. Execution: 1/01/22 → 30/06/25.
Phase Ib to evaluate safety of TAR-NK cells+cetuximab+irinotecan rechallenge in patients with mCRC (CITRIC-NK). Aura Muntasell Castellvi (PI, IMIM). Proyectos de Investigación Clínica Independiente (ICI) - Instituto de Salud Carlos III (ISCIII), Ref. CI24/00041. Execution: 01/01/25 → 31/12/2028.
Articles
Overcoming TGFβ and activin A suppression boosts NK cell antitumor function. Nat Immunol 26, 540–541 (2025).
Rea, A., Santana-Hernández, S., Villanueva, J. et al. Enhancing human NK cell antitumor function by knocking out SMAD4 to counteract TGFβ and activin A suppression. Nat Immunol (2025).
Santana-Hernández S, Suárez J, Servitja S, Berenguer-Molins P, Costa-Garcia M, Comerma L, Rea A, Perera J, Menéndez S, Arpí O, Bermejo B, Martínez-Larrad MT, Cejalvo JM, Comino-Méndez I, Pascual J, Alba E, López-Botet M, Rojo F, Rovira A, Albanell J, Muntasell A*. NK cell-triggered CCL5/IFNγ-CXCL9/10 axis underlies the clinical efficacy of neoadjuvant anti-HER2 antibodies in breast cancer. J Exp Clin Canc Res 2024; 43(1): 10.
López-Botet M*, De María A, Muntasell A, Della Chiesa M, Vilches C. Adaptive NK cell response to human cytomegalovirus: Facts and open issues. Semin Immunol 2023; 65: 101706.
Cabo M, Santana-Hernández S, Costa-Garcia M, Rea A, Lozano-Rodríguez R, Ataya M, Balaguer F, Juan M, Ochoa MC, Menéndez S, Comerma L, Rovira A, Berraondo P, Albanell J, Melero I, López-Botet M, Muntasell A. CD137 costimulation counteracts TGF? inhibition of NK-cell antitumor function. Cancer Immunol Res 2021; 9(12): 1476-1490.
Muntasell A*, Servitja S, Cabo M, Bermejo B, Perez-Buira S, Rojo F, Costa-Garcia M, Arpí O, Moraru M, Serrano L, Tusquets I, Martínez MT, Heredia G, Vera A, Martínez-García M, Soria L, Comerma L, Santana-Hernández S, Eroles P, Rovira A, Vilches C, Lluch A, Albanell J*, López-Botet M. High numbers of circulating CD57+ NK cells associate with resistance to HER2-specific therapeutic antibodies in HER2+ primary breast cancer. Cancer Immunol Res 2019; 7(8): 1280-1292.
Ochoa MC, Perez-Ruiz E, Minute L, Oñate C, Perez G, Rodríguez I, Zabaleta A, Alignani D, Fernandez-Sendin M, Lopez A, Muntasell A, Sanmamed MF, Paiva B, López-Botet M, Berraondo P, Melero I*. Daratumumab in combination with urelumab to potentiate anti-myeloma activity in lymphocyte-deficient mice reconstituted with human NK cells. OncoImmunology 2019; 8(7): 1599636.
Muntasell A*, Rojo F, Servitja S, Rubio-Perez C, Cabo M, Tamborero D, Costa-Garcia M, Martínez-García M, Menéndez S, Vazquez I, Lluch A, Gonzalez-Perez A, Rovira A, López-Botet M, Albanell J*. NK cell infiltrates and HLA class I expression in primary HER2+ breast cancer predict and uncouple pathological response and disease-free survival. Clin Cancer Res 2019; 25(5): 1535-1545.
Costa-García M, Ataya M, Moraru M, Vilches C, López-Botet M, Muntasell A*. Human Cytomegalovirus Antigen Presentation by HLA-DR+ NKG2C+ Adaptive NK Cells Specifically Activates Polyfunctional Effector Memory CD4+ T Lymphocytes. Front Immunol 2019; 10: 687.
Tamborero D*, Rubio-Perez C, Muiños F, Sabarinathan R, Piulats JM, Muntasell A, Dienstmann R, López-Bigas N, Gonzalez-Perez A*. A pan-cancer landscape of interactions between solid tumors and infiltrating immune cell populations. Clin Cancer Res 2018; 24(15): 3717-3728.
Cabo M, Offringa R, Zitvogel L, Kroemer G, Muntasell A*, Galluzzi L*. Trial Watch: Immunostimulatory monoclonal antibodies for oncological indications. OncoImmunology 2017; 6(12): e1371896.
Sabbaghi MA, Gil-Gómez G, Guardia C, Servitja S, Arpí O, García-Alonso S, Menéndez S, Arumí M, Serrano L, Salido M, Muntasell A, Martínez-García M, Zazo S, Chamizo C, González-Alonso P, Madoz-Gúrpide J, Eroles P, Arribas J, Tusquets I, Lluch A, Pandiella A, Rojo F, Rovira A, Albanell J*. Defective cyclin B1 induction in trastuzumab-emtansine (T-DM1) acquired resistance in HER2-positive breast cancer. Clin Cancer Res 2017; 23(22): 7006-7019.
Muntasell A*, Cabo M, Servitja S, Tusquets I, Martínez-García M, Rovira A, Rojo F, Albanell J, López-Botet M. Interplay between Natural Killer Cells and Anti-HER2 Antibodies: Perspectives for Breast Cancer Immunotherapy. Front Immunol 2017; 8: 1544.
López-Montañés M, Alari E, Sintes J, Martínez-Rodríguez JE, Muntasell A*, López-Botet M*. Antibody-Dependent NK Cell Activation Differentially Targets EBV-Infected Cells in Lytic Cycle and Bystander B Lymphocytes Bound to Viral Antigen-Containing Particles. J Immunol 2017; 199(2): 656-665.
Muntasell A, Ochoa MC, Cordeiro L, Berraondo P, López-Díaz de Ceiro A, Cabo M, López-Botet M, Melero I*. Targeting NK-cell checkpoints for cancer immunotherapy. Curr Opin Immunol 2017; 45: 73-81.
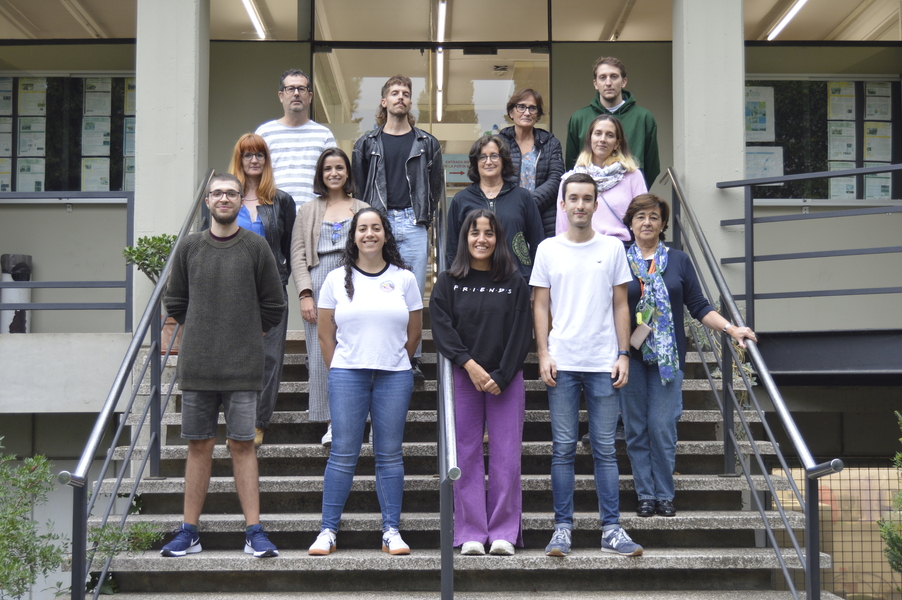
Team members
Predoctoral Researcher: Santana Rodríguez, Sara
Predoctoral Researcher: Villanueva Iglesias, Javier
Postdoctoral Researcher: Gardeta Castillo, Sofia
Collaborators
Joan Albanell. Head of the Oncology Service of the Hospital del Mar. Head of the Molecular Cancer Therapy Laboratory
Clara Montagut. Coordinator of the Colorectal Cancer Precision Medicine Group
Ana Rovira. Coordinator of the Molecular Cancer Therapy Laboratory
Anna Hernández. Head of the Molecular Cancer Therapy Laboratory
Fabricio Quimis. Laboratory Technician
More information
Principal investigator
Aura Muntasell, PhD. Lecturer Serra Hunter at the Autonomous University of Barcelona. Senior researcher of the research group in molecular cancer therapy at the Hospital del Mar Research Institute. Senior researcher in the Cellular Immunology group of the Institute of Biotechnology and Biomedicine.
Information of interest
PAPEL DE LAS ALTERACIONES DE LA PRESENTACION DE ANTIGENO MEDIADAS POR STRESS EN CELULAS BETA Y EN EL DESARROLLO DE LA DIABETES DE TIPO 1. Carme Roura Mir (PI), M.D. Jaraquemada Perez de Guzman. Convocatòria Proyectos de Generación del Conocimiento (Ref. PID2021-125470OB-I00). Ministerio de Ciencia e Innovación. Execution: 1/09/22 → 31/08/25.
Roura-Mir, C., Catalfamo, M., Cheng, TY, Marqusee, E., Besra, GS, Jaraquemada, D. i Moody, DB (2005) Journal of Immunology 174, 3773-3780.
Blanco, Y., Saiz, A., Costa, M., Torres-Peraza, J.F., Carreras, E., Albrech, J., Jaraquemada, D. i Graus, F. (2005) Neuroscience Letters 380, 122- 126.
Saiz, A., Carreras, E., Torres-Pefaza, J., Costa, M., Alberch, J., Jaraquemada, D. i Graus, E. (2004) Multiple Sclerosis 10, S168-S168.
Muntasell, A., Carrascal, M., Alvarez, I., Serradell, L., van Veelen, P., Verreck, FAW, Koning, F., Abian, J. i Jaraquemada, D. (2004) Journal of Immunologia 173, 1085-1093.
Garavito, G., Yunis, EJ, Egea, E., Ramírez, LA, Malagon, J., Iglesias, A., De La Cruz, OF, Uribe, O., Navarro, E., Martinez, P. i Jaraquemada, D. (2004) Immunologia humana 65, 359-365.
Diaz, G., Amicosante, M., Jaraquemada, D., Butler, RH, Guillen, MV, Sanchez, M., Nombela, C. i Arroyo, J. (2003) International Immunology 15, 565-576.
Muntasesll, A., Carrascal, M., Serradell, L., van Veelen, P., Verreck, F., Koning, F., Raposo, G., Abian, J. i Jaraquemada, D. (2002) Journal d'Immunologia 169, 5052-5060.
Fernandez-Mestre, MT, Jaraquemada, D., Bruno, RE, Caro, J. i Layrisse, Z. (2002) Tissue Antigens 60, 10-15.
Dodi, IA, Van Rhee, F., Forde, HC, Roura-Mir, C., Jaraquemada, D., Goldman, JM i Madrigal, JA (2002) Cytotherapy 4, 353-363.
Costa, M., Saiz, A., Casamitjana, R., Castaner, MF, Sanmarti, A., Graus, F. i Jaraquemada, D. (2002) Clinical and Experimental Immunology 129, 471-478
Funding
Additional information