Knowing the individual genetic variants to personalize the treatment for childhood leukemia
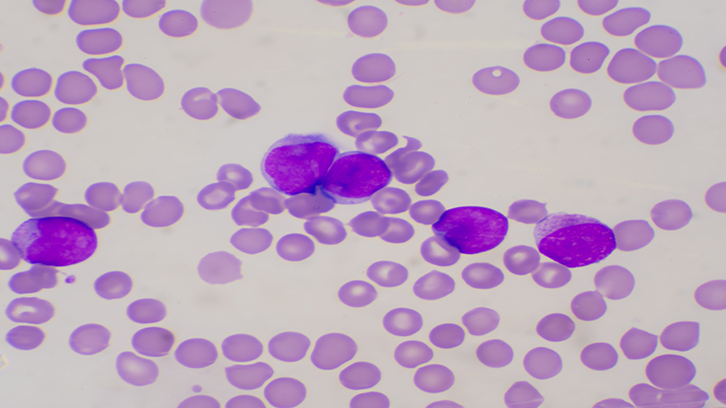
Individualization of treatment for Acute Lymphoblastic Leukemia is key to improving survival for patients with this disease, which accounts for one third of all childhood cancers. This study analyzed genes involved in the death of cancer cells, and found an association between the presence of genetic variants in these genes and the survival of patients. If these results are confirmed in a broader series of patients, those individuals at high risk for resistance to chemotherapy agents based on programmed cell death (apoptosis) could be identified, so they could be treated with other, more aggressive therapies.
Acute lymphoblastic leukemia (ALL) is the most common cancer in children, representing one third of all childhood malignancies. Progressive intensification of multiple drug chemotherapeutic regimens has improved outcomes for children with ALL; however, up to 20% of patients relapse, and have poor prognosis. Identification of children with ALL that have poor response to chemotherapy is important to individualize therapy. Inherited genetic variation may partially explain why children with ALL respond differently to chemotherapy. Scientists have searched clinically useful genetic predictors of ALL treatment response, by studying variants at different candidate genes; however, despite extensive analysis, the underlying genetic variants responsible for differences in ALL outcome have remained elusive.
In the present study, our group (Unit of Biological Anthropology, Faculty of Biosciences, UAB) searched whether variations in genes coding for proteins involved metabolism of chemotherapy agents or in progammed cell death (apoptosis) had an impact on the therapeutic outcome of childhood ALL patients. We investigated the association between genetic variants in five genes and treatment response, relapse and patient survival in 173 children with ALL from Hospital Sant Joan de Déu and Hospital Vall d’Hebron from Barcelona. After the analysis, we observed that there was a significant association between variants in two genes involved in apoptosis (GSTM1 and TP53) and patient survival. Specifically, patients having the genotype GSTM1 non-null and TP53 Pro at codon 72 presented a highly significant reduction of survival (p=0.0005). Moreover, we confirmed these results in vitro on leukemic cells treated with a chemotherapy agent: a glucocorticoid. Glucocorticoids are the keystone in the treatment of childhood ALL due to their ability to induce extensive apoptosis in ALL cells. Leukemic cells with this specific genotype at GSTM1 and TP53 exhibited the lowest sensitivity to the drug compared to cells with other genotypes.
Therefore, we concluded that having this specific genotype at GSTM1 and TP53 would lead to less efficient apoptosis of ALL lymphoblasts after anti-leukemic treatment and this could translate into shorter survival of patients, contributing to differences in response to therapy in childhood ALL.
Our study, if confirmed in larger series, may provide tools to individualize drug therapy in childhood ALL. Patients with a specific genotype at GSTM1 and TP53 could be identified as having a high risk of resistance to apoptotic-based agents and could benefit from other more aggressive therapies.
Departament de Biologia Animal, Biologia Vegetal i Ecologia
Facultat de Biociències
Universitat Autònoma de Barcelona
References
Cabezas M, Camós M, Rives S, Garcia-Orad A, Lopez-Lopez E, Dapena JL, Caballín MR, Armengol G. Impact of polymorphisms in apoptosis-related genes on the outcome of childhood acute lymphoblastic leukaemia. Br J Haematol. 2019 Apr;185(1):159-162. doi: 10.1111/bjh.15415.

