The main cause of vertigo can be easily diagnosed and treated by primary care physicians
Patients who experience vertigo, which is typically described as a dizzy feeling, often seek emergency care at their local hospital or primary healthcare center. Dizziness is the main symptom described in up to 5% of all outpatient consultations and the most common cause is vertigo. Patients with vertigo feel as if the things around them or they themselves are spinning.
The most common form of vertigo is posterior canal Benign Positional Paroxysmal Vertigo (BPPV), which can cause considerable anxiety as simple movements like turning over or getting out of bed can send the room spinning. The sensation is short-lived, but it returns as soon as the patient attempts to move again. In addition, it is often accompanied by nausea and even vomiting.
Concerned about this unpleasant and often frightening condition, patients tend to seek emergency care. BPPV also has a considerable impact of quality of life, with two out of every three patients either stopping work or cutting back on hours. Although 50% to 70% of patients with BPPV improve within a month (with or without treatment), the condition can last for months or even years.
BPPV is caused by a problem in the semicircular canals, which are three tiny tubes located in the inner ear. These canals help control balance and contain a gelatinous substance known as endolymph. Their sensitivity is altered by the displacement of calcium carbonate crystals normally attached to another part of the inner ear into the canals, triggering the symptoms of BPPV. The posterior canal is the most frequently involved of the three canals.
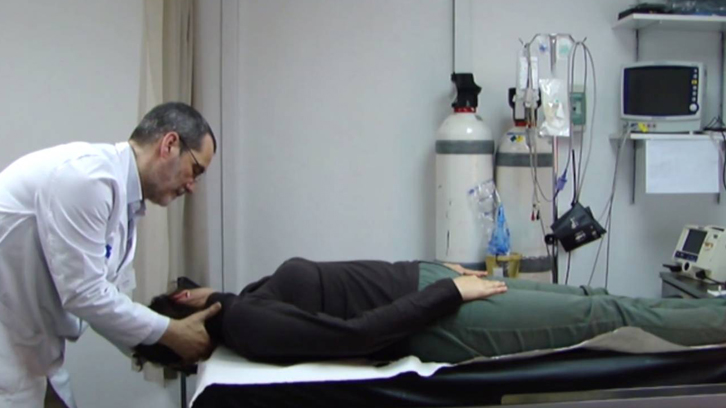
BPPV can be diagnosed using a simple physical maneuver that can be performed by a family physician without the need for specific equipment or for blood tests, X-rays, or other tests. This maneuver is called the Dix-Hallpike test and is shown in the following video.
A diagnosis of typical or objective BPPV is made when the Dix-Hallpike test causes both vertigo and repeated, uncontrolled eye movements known as nystagmus. These movements explain why the patient feels that everything around him or her is spinning. When nystagmus is not observed but the patient experiences vertigo, a diagnosis of subjective BPPV is made.
BPPV can also be treated with a very simple physical maneuver that takes just 2 minutes and can be also by performed by family physicians. The purpose of the maneuver is to reposition the dislodged calcium crystals in the semicircular canals. This repositioning technique is known as the Epley maneuver and is explained in the following video.
Although the Epley maneuver is very simple and highly effective (almost 100% of patients recover after undergoing the procedure up to 4 times), it is not routine practice in either primary healthcare or hospital emergency settings, which is where most of these patients are seen. Many patients with BPPV therefore are not properly diagnosed or treated. One of the reasons why the Dix-Hallpike and Epley maneuvers are not routinely used in these settings is that most studies to date have analyzed their use in specialized settings equipped with instruments to aid detection of nystagmus.
Our team designed a study to test whether family physicians could successfully use these two simple maneuvers to diagnose and treat BPPV after just a 2-hour training session. The study was a clinical trial in which 134 patients with subjective and objective BPPV were randomly assigned to be treated with either the Epley maneuver or a sham procedure designed to mimic this maneuver. All the patients were additionally prescribed betahistine, which is the main drug used to treat BPPV worldwide.
The doctors responsible for assessing the patients did not know whether they had been treated with the Epley or the sham maneuver. At the follow-up visits, held a week, a month, and a year after treatment, the patients were administered the Dix-Hallpike test and asked to rate the severity of their vertigo on a scale of 1 to 10. They were also asked whether their vertigo had cleared up completely or not.
The improvements were evident in the patients diagnosed with objective BPPV (vertigo and nystagmus) in the initial Dix-Hallpike test. Those treated with the Epley maneuver were six times more likely than those treated with the sham maneuver to test negative for BPPV in the follow-up Dix-Hallpike tests. Self-reported symptom severity also improved by an average of 2 points in this subgroup of patients. The only variable that did not vary significantly between any of the subgroups analyzed was the question on whether their vertigo had completely disappeared. We believe that this is because patients successfully treated with the Epley maneuver may continue to experience mild dizziness for some time. One study in particular found that this was the case for two-thirds of patients. It is thus difficult to detect differences based on a simple yes/no question.
No significant improvements were observed in the almost 60% of patients with subjective BPPV (vertigo only) in our study. Nystagmus, however, can be difficult to detect without the help of specialized instruments, and it may be therefore that they had other types of vertigo. Diagnosis in primary healthcare settings could probably be improved through training in observation techniques and access to equipment such as Frenzel goggles (they allow seeing nystagmus more easily).
Another potential limitation of our study is that patients in both the treatment and sham groups were prescribed betahistine, which could have made improvements due exclusively to the Epley maneuver more difficult to detect. Not giving the patients in the sham group treatment, however, was not an option as the study lasted for a year.
We believe that there is no reason not to treat suspected BPPV with the Epley maneuver in routine practice, as it takes just 2 minutes, costs practically nothing, and is very safe. The only adverse effect observed in our study was nausea, reported by 13% of the patients in the Epley maneuver group.
In short, we hope that the results of our study will encourage family physicians all over the world to use these two simple procedures to diagnose and treat BPPV as part of everyday practice. As they gain experience, they will become better at detecting nystagmus, which should result in more effective diagnosis and treatment. With a little more training, they could also treat horizontal canal BPPV, which accounts for 10% to 15% of all cases of BPPV and is diagnosed and treated with similar maneuvers to those used in posterior canal BPPV.
Advances in this area will probably improve the quality of life of patients with BPPV, enable a faster return to work, and significantly reduce falls, particularly in seniors. These and other aspects of BPPV could be the focus of new epidemiological studies of this common disorder.
Figure 1. General outline of the study.
Universitat Autònoma de Barcelona
References
Ballve JL, Carrillo R, Rando Y, Villar I, Cunillera O, Almeda J, Rodero E, Monteverde X, Rubio C, Moreno N, Arias OL, Martin C, Azagra R. (2019). Effectiveness of the Epley manoeuvre in posterior canal benign paroxysmalpositional vertigo: a randomised clinical trial in primary care. Br J Gen Pract, 69(678):e52-e60. DOI: 10.3399/bjgp18X700253.


