Medicine and Health
Twins born with no hereditary pathology
For the first time ever, the birth of a boy and a girl without the monogenic hereditary non polyposis colon-rectal cancer (HNPCC) disease or Lynch Syndrome, present in the father has been achieved. This was been possible after a successful application of Preimplantation Genetic Diagnosis for Double Genetic factor (DF-PGD). This research was developed for a team in the Unitat de Biologia Cel·lular i Genètica Mèdica de la Facultat de Medicina de la UAB formed by MSc G. Daina, MSc L. Ramos, Dra. M. Rius, Dr. A. Obradors, Dr. J. del Rey, Dr. J. Benet, and leaded by Dra. Joaquima Navarro and in collaboration with a team from the Puigvert-Hospital de la Santa Creu i Sant Pau Foundation formed by Dra. Polo y la Dra. O. Martínez Passarell, leaded by Dr. J. Calaf and with Dr. J. Obradors from the Consultori Obstètrico i Ginecològic Josep Obradors and with Dr. J. Brunet del Servicio de Oncologia Médica de ICO de Girona.
References
“First successful double-factor PGD for Lynch Syndrome: monogenic analysis and comprehensive aneuploidy screening”. Clinical Genetics (Daina i col.,). DOI: 10.1111/cge.12025
The monogenic hereditary non polyposis colon-rectal cancer (HNPCC) disease or Lynch Syndrome is manifested in the 80% of the afected by the mutation and frequently affects DNA repair genes, which are important in maintaining genomic stability during DNA replication. With 655,000 deaths a year worldwide, it is the fourth most common cancer in the United States and the third leading cause of cancer-related deaths in Western countries.
According to data from the European Society of Human Reproduction and Embryology (ESHRE), the PGD process results in pregnancy in about 14% of embryos free of familial mutation transferred to the uterus. One reason for this low implantation rate may be due to the existence of chromosome alterations (aneuploidy) in transferred embryos. In cycles of PGD for monogenic diseases chromosome abnormalities present in the embryo are, usually, not analysed.
In the DF-PGD developed at the UAB, in addition to the mutation responsible for family monogenetic diseases, all chromosomes (chromosomes 1-22, X and Y) of evolved embryos are analysed. It also has the advantage that both results are achieved on four days which allows for embryo selection and transfer to the uterus without freezing them.
In this case, the selection of embryos not only not affected by Lynch Syndrome but also chromosomally normal for all of the chromosomes, was performed in collaboration with the Programa de Reproducció Assistida de la Fundació Puigvert–Hospital de la Santa Creu i Sant Pau where the whole assisted-reproduction techniques were performed.
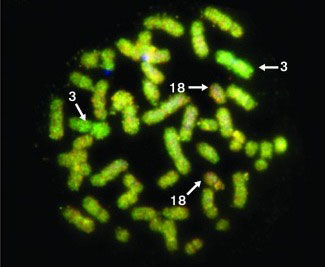
So, on three days' evolved embryos, two embryonic cells were extracted. One of them was used for the study the hereditarian mutation and the other was used for the study of the full complement of chromosomes (chromosomes 1-22, X and Y) using the rapid Comparative Genomic Hybridization (CGH) developed in our group, which uses MetaSystems software (IZASA).
Successful mutation analysis was obtained in 12 out of the 14 evolved embryos biopsied (85.7%) with 5 being (41.7%) healthy embryos without the mutation, and 3 of them were diagnosed as being chromosomally normal.
Two of these embryos were transferred to the uterus in five days resulting in the birth of a boy and a girl, both being negative healthy for Lynch syndrome, of which the postnatal genetic diagnosis was concordant with the results obtained in DF-PGD.
DF-PGD may be a useful tool to select embryos free of monogenic diseases and chromosomally normal allowing for the improvement of the implantation rate of transferred embryos.
Joaquima Navarro
Department of Cellular Biology, Physiology and Immunology
2026 Universitat Autònoma de Barcelona
B.11870-2012 ISSN: 2014-6388
